The I AM Project aims to implement a more sustainable and accurate screening process at Prince of Wales Hospital for patients who are malnourished, or at risk of malnutrition.
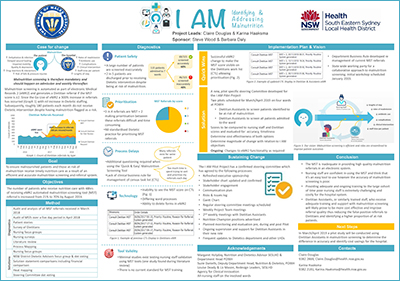
View a poster from the Centre for Healthcare Redesign graduation, December 2018.
Aim
To improve the accuracy of malnutrition screening at Prince of Wales Hospital from 43% to 80% by August 2019.
Benefits
If malnutrition, or the risk of becoming malnourished, is identified and addressed in a timely manner, there can be many positive outcomes for both the patient and the health system.
For the individual
- Improved wound healing
- Reduced risk of falls and pressure injuries
- Reduced muscle wasting and weakness
- Reduced prevalence of adverse drug reactions and drug interactions
- Reduced infection rates
- Improved hydration
- Reduced diarrhoea and constipation
- Improved metabolic profiles
- Reduced apathy and depression1
For the health system
- Reduced length of stay
- Reduced antibiotic use
- Reduced clinical complications
- Reduced staff time per patient
- Reduced rates of readmission
- Reduced healthcare costs1
Background
In June 2017, the malnutrition screening process for patients at Prince of Wales Hospital changed from a paper to an electronic form which automated the referral. The Malnutrition Screening Tool (MST) is completed by nursing staff when a patient is admitted to the hospital, and weekly thereafter. If a patient is identified to be at risk of malnutrition (MST score ≥ 2) a referral is sent to the dietitian’s task list.
The automation of this referral process resulted in a 300% increase in referrals to dietitians. However, there was no increase in staffing to manage the demand and many patients who were identified to be at risk of malnutrition were not seen. Roughly 180 patients were discharged each month without receiving any dietetic intervention.
Not only was the number of referrals coming through the system increasing, it also become more difficult to differentiate the higher priority referrals. The MST tool provides a score from 0-5 with a score of greater than 2 identifying malnutrition risk. Preliminary research showed that 75% of the referrals received had a MST score of 2 making it difficult to prioritise these patients when/if able.
Implementation
A pilot study will be conducted at Prince of Wales Hospital during March/April 2019 to support the proposed changes to the current nutrition screening process. As dietitian assistants are a much smaller workforce than nursing staff, they could receive training and supervision from dietitians for malnutrition screening as part of their daily workload.
The pilot study will consist of two different streams:
- The dietitian assistant performs all malnutrition screening for newly admitted patients admitted to Prince of Wales Hospital (within four selected wards).
- Nursing staff continue to screen patients on admission however dietitian assistants will re-screen low-risk patients (MST=2).
During the two streams of the pilot, the nursing staff MST score and the dietitian assistant MST score will be compared with the dietitian MST score. This will then be analyzed to determine which stream is better able to improve nutrition screening and contribute to a more sustainable and accurate screening process. Post-pilot evaluation, clinical business rules will be developed for dietitian assistants and dietitians, outlining the new process for malnutrition screening to support solution sustainability.
Status
Future initiative – The project is in the operational plan or is an active work project.
Dates
26 March 2018 to 31 May 2019
Implementation sites
This project will be piloted in March 2019 on the cardiac and respiratory wards at the Prince of Wales Hospital. The implementation will involve various stakeholders and staff members from various teams including nursing staff, dietitian assistants, dietitians and information technology staff.
Partnerships
Centre for Healthcare Redesign, Agency for Clinical Innovation
Evaluation
Currently, the project team continues to meet weekly in the preparation for a pilot implementation project, due to go live in March 2019.
During the pilot period (March-April 2019) the project team will conduct an audit of all newly admitted patients to the cardiac and respiratory wards over a one week period. The MST score obtained by both nursing staff and dietitian assistants will be compared to the score obtained by the auditing dietitian as a reference standard.
During the five week pilot period, support sessions between dietitians and dietitian Assistants will be held frequently to identify and discuss barriers and enablers in the screening process.
Following the pilot period (April 2019), surveys and discussion groups will be held with dietitian assistants to review the screening process, determine the success of the solution, and discuss how the screening process can be further improved for implementation throughout the hospital.
Lessons learnt
It was important to engage nursing staff from each ward throughout the whole re-design process. Active participation within focus groups and brainstorming activities ensured that all voices, problems and issues were heard and could be included in solution design and implementation planning.
Having a member from the information technology team on the steering committee proved useful and this member was able to provide insights we otherwise would have been oblivious to. Unfortunately this team member left the organisation and was not able to be replaced within the steering committee which slowed down the implementation of quick wins.
The Nursing Education and Research Unit (NERU) was contacted during implementation planning however in hindsight this staffing group would have been beneficial to involve during solution design.
References
- NSW Ministry of Health. Nutrition Care PD2017_041. [Internet]. 2017 [cited 2018 March 1].
Further reading
- Bell J, Bauer J, Capra S. The malnutrition screening tool versus objective measures to detect malnutrition in hip fracture. J of Hum Nutr Diet. 2013:26(6):519-526.
- Ferguson M, Capra M, Bauer J, Banks M. Development of a Valid and Reliable Malnutrition Screening Tool for Adult Acute Hospital Patients. Nutrition. 1999:15(6):458-464.
- Marshall S, Young A, Isenring E. The malnutrition screening tool in geriatric rehabilitation: A comparison of validity when completed by health professionals with and without malnutrition screening training has implications for practice. Bond University: bepress. 2017. Available from: https://pubmed.ncbi.nlm.nih.gov/28476323
- Phillips W, Zechariah S. Minimizing False-Positive Nutrition Referrals Generated from the Malnutrition Screening Tool. Journal of the Academy of Nutrition and Dietetics. 2017:117(5):665-669.
- Wester P, Angus R, Easlea D, et al. Use of the malnutrition screening tool by non-dietitians to identify at-risk patients in a rehabilitation setting: A validation study. Nutr Diet. 2018. In print. DOI: 10.1016/j.jand.2017.03.019.
- Wu M, Courtney M, Shortbridge-Bagget L, et al. Validity of the malnutrition screening tool for older adults at high risk of hospital readmission. J Gerontol Nurs. 2012:38(6):38-45.
Contacts
Karina Haaksma
Clinical Dietitian
Prince of Wales Hospital
Phone: 02 9382 2880
Karina.Haaksma@health.nsw.gov.au
Claire Douglas
Clinical Dietitian
Prince of Wales Hospital
Phone: 02 9382 2880
Claire.Douglas@health.nsw.gov.au