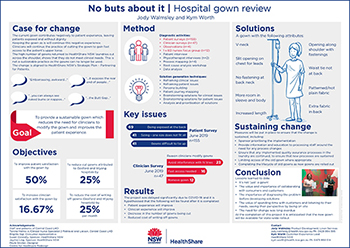
This project looked at how the most common hospital gown used in NSW public hospitals could be improved for patients, clinicians and the health system.
Patients report that the hospital gown is unsuitable mostly due to the lack of modesty it provides. The gown does not meet the needs of clinicians, as it can interfere with intravenous lines and does not provide access to the patient’s upper torso. It is often cut across the shoulder to accommodate clinical needs, and this in turn, leads to excessive replacement costs. This project set out to design a sustainable gown providing an improved patient experience which also meets the needs of clinicians.
Aim
To provide a sustainable gown to five wards at Gosford and Wyong hospitals, which:
- improves patient satisfaction with the gown by 50% within six months
- improves clinician satisfaction by 16% within six months
- decreases the number of clinician-modified gowns by 16% within six months
- reduces the cost of writing off gowns by 25%, within six months.
Benefits
Delivery of the project goal and objectives may also result in the following additional benefits.
Patients
- Patients are better covered and feel less exposed.
- Patients feel less institutionalised.
- Reduced risk of pressure injuries caused by knots, less associated time in hospital.
Staff
- Don’t need to cut the gown, therefore saving time and decreasing waste.
- Knowledge of patients feeling covered.
- A gown that is fit for purpose.
System
- Availability of a gown for statewide rollout.
- Benefits of a sustainable gown including less waste and longer lifecycle.
- Better placed to review gown offerings.
Program status
Program dates
- April 2019 – present.
The project has been delayed due to COVID-19.
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Background
The way patients in NSW feel when they go to hospital and put on a gown has never been considered in the design of the gown. There are several reasons for this, including the historical lack of patient centricity, innovation and the operational environment of the linen service.
It was identified at Newcastle Linen Service that a high number of gowns returned to the laundry had been cut across the shoulder. These gowns were no longer able to be used. The negative cost effect cost to Newcastle Linen Service due to writing off gowns was $2926 + GST per month. The state-wide cost would be significantly more.
It was not immediately clear why so many gowns were being cut across the shoulder. There was also no deep understanding of what the elements of a fit for purpose gown would be from a clinician perspective, or what a patient centred gown would include. Investigations needed to be carried out to determine answers to these questions.
Implementation
Diagnostic activities were undertaken to determine the key issues with the gown for patients and clinicians. These included surveys, observations, process mapping, a focus group, a patient interview, data analysis and root cause analysis.
For patients the gown did not provide modesty due to the back opening. Sizing was an issue, and patients reported difficulty in doing the gown up without help. Patient satisfaction with the gown was low at 4.4/10.
For clinicians the gown did not meet their needs as it interfered with IV lines and did not provide access to the patient’s upper torso, resulting in it often being cut across the shoulder. Knots and folds in the back of the gown can put pressure on the patient’s body.
In July 2019 the solution ideas to address the issues above were determined using several techniques, including the following.
- Reframing of the three identified clinical issues into two issues in the frame of reference of clinicians. This helped to understand from their perspective, leading to solutions that are better designed to meet their needs.
- Reframing the three identified patient issues into the frame of reference of the patient. This helped to understand the issues from their perspective, leading to patient-centred solutions.
- A persona building exercise, where a patient persona, ‘Bob’, was created. This helped to develop empathy with the patient and a better understanding of what matters to them, leading to solutions that better meet their needs and improve the patient experience.
- The patient journey was mapped throughout their hospital experience. This exercise discovered pain points and moments that matter for the patient, as well as a better understanding of what needs to be focussed on to improve the patient experience.
- Brainstorming with Clinical Nurse Consultants which led to several ideas for various aspects of the gown.
- Brainstorming with Linen Operations Managers, which helped identify possible solutions from a linen processing perspective.
- Ideas provided by patients during the diagnostics phase were withheld until the solutions phase when they were analysed and prioritised.
- Brainstorming solutions with the linen supplier.
The solution generating exercises found that a suitable gown would include the following elements:
- coloured and possibly patterned fabric
- attention to the fabric used (subject to testing)
- v-shaped neckline
- no fastening at the back of the neck
- wider sleeve
- openings along each shoulder with fastenings
- more room in the body
- increased length
- waist tie that ties towards the front.
An experienced designer was engaged to develop gown prototypes.
Completion of the project has been delayed due to COVID-19. Testing of prototypes will be conducted with patients, clinicians, and the laundry process.
Upon completion of testing, a gown will be trialled in wards at Gosford and Wyong hospitals.
Implementation sites
This project will be implemented in five wards and departments in Central Coast Local Health District.
- Gosford Hospital: theatres, intensive care unit.
- Wyong Hospital: emergency department, surgical assessment centre, S1 surgical ward.
Partnerships
- Centre for Healthcare Redesign
- Central Coast Local Health District
Results
Evaluation will take place in the second half of 2021.
The following evaluation measurements will be compared with baseline measures.
- Patient and clinician surveys to measure satisfaction with the gown.
- Measure decreases in clinician-modified gowns.
- Measure the cost of writing off gowns.
Lessons learnt
- It’s not ‘just’ a gown!
- The importance of collaborating with customers.
- The importance of diagnosing the problem, not jumping to solutions.
- The value of spending time with customers and listening to their needs.
- The value of understanding the customer perspective by seeing it first hand in their environment - being on site.
- The range of stakeholders is broader than initially realised.
- The importance of consumer involvement.
- The need for change was long overdue.
- The importance of planning and communication.
Contacts
Jody Walmsley
Linen Product Development Supervisor
HealthShare NSW
Phone: 0429 994 595
jody.walmsley@health.nsw.gov.au
Kym Worth
Customer Experience Lead
HealthShare NSW
Phone: 0475 950 514
kym.worth@health.nsw.gov.au