Our project identified our patients are worried about access to, and the quality of, care they receive. Our staff want to work collaboratively and partner with patients to provide timely, high quality, integrated healthcare. The project has provided impetus for patients to be active participants in their care and for staff to move away from providing siloed healthcare and create an integrated healthcare experience for our patients.
View a poster from the Centre for Healthcare Redesign graduation December 2021.
Aim
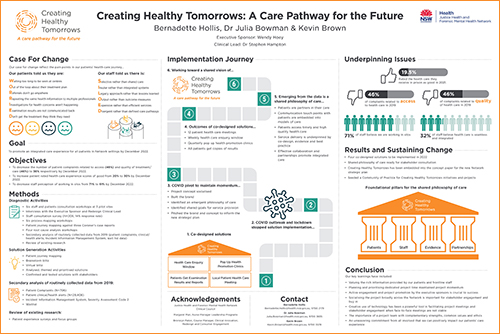
The goal of the project is to promote an integrated care experience for all patients in Justice Health and Forensic Mental Health Network (JHFMHN) settings by December 2022.
This will be measured by:
- decreasing the number of patient complaints related to access (46%) and quality of treatment or care (46%) to 36% respectively by December 2022
- increasing patient rated healthcare experience scores of ‘excellent’ or ‘very good’ from 27% to 37% by December 2022
- decreasing staff perception of working in silos from 71% to 61% by December 2022.
Benefits
Our patients will have:
- a voice and opportunity to raise concerns
- access to their health information and will be partners in their health planning
- improved access to clinicians
- scheduled access to health promotion and health screening.
Our staff will have:
- the opportunity to work collaboratively with other service providers
- input into how healthcare is provided to our patients
- a mechanism to co-design the way care is provided.
Our organisation will have:
- a clear, overarching care philosophy guiding strategic planning for the future
- a structure to guide the development of models of care
- service delivery models focused on patient-centred care.
Background
JHFMHN is a statewide service that provides healthcare to adults and young people in contact with the criminal justice and forensic mental health systems in NSW (secure settings). We are a healthcare organisation working in environments across the state governed by Department of Community and Justice NSW, apart from the Forensic Hospital, which is solely under the jurisdiction of NSW Health. Inmates in our care are referred to as patients.
Forty one percent of adults in secure settings have complex health needs. That is, they experience a combination of multiple chronic conditions, mental health problems, drug interactions and various social vulnerabilities.2
This project is focused on the most important person in healthcare, the patient. Whilst JHFMHN’s vision is to return healthier patients to their communities, after recent reflection, and review by senior stakeholders, it was agreed that despite the work that has been undertaken to develop models of care for clinical specialties, the overall healthcare journey for patients is inconsistent, siloed and not well integrated.3 This has the potential to introduce safety and quality of care issues for our patients.4,5 Further, a silo mentality compromises organisational efficiency, promotes conflicts, and causes redundancy and waste. This serves to distress and demotivate employees and frustrate patients who receive suboptimal care and do not have their healthcare needs met in a timely manner.6
Implementation
Regular engagement and consultation with our stakeholders led to the co-design of five solutions for implementation. Implementation of solutions has been postponed until 2022 due to the impact of the COVID-19 pandemic.
Solution 1: Change the COVID-19 Temperature Check Guidelines
Amend the JHFMHN COVID-19 Temperature Checking Guidelines to reflect that all health professionals must take the temperature of their own patients on entry to the health centre prior to the consultation commencing.
Solution 2: Introduce a local patient and health service interface meeting to improve communication between patients and clinicians
This meeting will be introduced at our pilot sites by the Patient Health Care Committee. It is intended to improve communication between patients and healthcare providers at the secure setting where they are housed.
Solution 3: Creation of a health enquiry window
The health enquiry window will run twice per week for patients at each health centre. Patients can have a face-to-face conversation with health centre staff, without a self-referral, to make enquiries about healthcare issues of concern to them.
Solution 4: Pop-up health clinics
Quarterly pop-up clinics to pilot sites and scaled up to all public correctional centres across NSW.
Solution 5: Copies of examination results provided to patients
Develop a new JHFMHN policy to outline the roles, responsibilities and practice behaviours for all parties to enable copies of reports and results to be given to the patient.
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
- Start date: February 2021
- End date: December 2022
Implementation sites
- Pilot site 1 – Dillwynia Correctional Centre
- Pilot site 2 – Metropolitan Specialty Programs Centre Area 3, Long Bay Correctional Complex
- Pilot site 3 – the Forensic Hospital
Partnerships
- Centre for Healthcare Redesign, Agency for Clinical Innovation
- Corrective Services NSW
Evaluation
Evaluation timelines have been pushed back as a result of the recent COVID-19 Delta outbreak and lockdown in NSW. Evaluation of all solutions will occur in 2022.
Solution 1: Change the COVID-19 Temperature Check Guidelines
- Change to the guideline.
- Change in clinical practice.
Solution 2: Introduce a local patient and health service interface meeting to improve communication between patients and clinicians
- Monthly meeting at all pilot sites.
- Scaled up to all centres and sites under the jurisdiction of JHFMHN.
Solution 3: Creation of a health enquiry window
- Twice-weekly enquiry window at all pilot sites.
- Scaled up to all correctional centres as fit for the environment.
Solution 4: Pop-up health clinics
- Quarterly pop-up clinics at all pilot sites.
- Scaled up to all correctional centres as fit for the environment.
Solution 5: Copies of examination results provided to patients
- Working with clinical directors, patients will receive their examination results and have the opportunity for a follow up discussion at all pilot sites.
- Scaled up to all correctional centres as fit for the environment.
Lessons learnt
- The value of the rich information provided by our patients and frontline staff.
- Dedicated project time.
- Regular meetings with and active engagement and promotion by with project sponsors.
- Support from the ACI is invaluable.
- The importance of socialising the project broadly across JHFMHN.
- Use technology to facilitate project meetings and stakeholder engagement when face-to-face meetings are not viable.
References
- Bujold M, Pluye P, Légaré F, et al. Decisional needs assessment of patients with complex care needs in primary care: A participatory systematic mixed studies review protocol. BMJ Open 2017;7:e016400. DOI: 10.1136/bmjopen-2017-016400
- Davidson P, Halcomb E, Hickman L, et al. Beyond the rhetoric: What do we mean by a ‘model of care’? Aust J Adv Nurs. Mar-May 2006;23(3):47-55.
- Lawal AK, Rotter T, Kinsman L, et al. What is a clinical pathway? Refinement of an operational definition to identify clinical pathway studies for a Cochrane systematic review. BMC Med. 2016 Feb 23;14:35. DOI 10.1186/s12916-016-0580-z.
- Varkey P, Reller MK, Resar RK. Basics of quality improvement in health care. Mayo Clin Proc. 2007 Jun;82(6):735-9. DOI: 10.4065/82.6.735.
- Meneses R, Caseirp J. Silos mentality in healthcare services. In: Vrontis D, Weber Y, Tsoukatos E, et al. editors. 11th Annual Conference of the EuroMed Academy of Business - Research Advancements in National and Global Business Theory and Practice: conference proceedings, vol 1 [Internet]; 2018 Sep 12-14; Valletta, Malta. Euromed Research Business Institute; 2018. Available from: https://emrbi.org/wp-content/uploads/2019/07/EuroMed-11-2018-SCOPUS.pdf
Further reading
- Justice Health and Forensic Mental Health Network
- United Nations Office on Drugs and Crime. The United Nations Standard Minimum Rules for the Treatment of Prisoners: (the Nelson Mandela Rules). V.16-00193. United Nations Office on Drugs and Crime; 2017.
- Royal Australian College of General Practitioners. Standards for health services in Australian prisons (1st ed.) [Internet]: Royal Australian College of General Practitioners; 2011.
Contacts
Bernadette Hollis
Nurse Manager Professional Practice
Justice Health and Forensic Mental Health Network
Bernadette.Hollis@health.nsw.gov.au
Dr Julia Bowman
Research Operations Manager
Justice Health and Forensic Mental Health Network
Julia.Bowman@health.nsw.gov.au
Kevin Brown
Manager Allied Health, Forensic Hospital
Justice Health and Forensic Mental Health Network
Kevin.Brown@health.nsw.gov.au